Ocular Surgery News U.S. Edition, November 10, 2019
Soosan Jacob, MS, FRCS, DNB; Amar Agarwal, MS, FRCS, FRCOphth
Keratoconus has been successfully treated with synthetic intrastromal corneal ring segments for many years now; however, there is an associated risk with implanting a synthetic substance within the cornea. With a complication rate of up to 30% reported in some series, many are hesitant to implant these devices despite the good outcomes with topography and vision.
One of the authors, Soosan Jacob, devised a technique called corneal allogenic intrastromal ring segments (CAIRS), which, as the name implies, refers to the use of allogenic tissue as intracorneal ring segments. The use of human stromal tissue eliminates many of the disadvantages that are associated with synthetic intrastromal corneal ring segments (ICRS) while having the advantage of improving topographic and visual outcomes.
Technique
Human donor corneal tissue is stripped of all epithelium and endothelium. It is then punched with a special trephine, designed by Jacob, that has two concentric blades. This allows punching of a circular segment of tissue, which is then cut into two halves. The segments are flattened and cut into appropriate size. Meanwhile, femtosecond-dissected channels are prepared in the keratoconic patient’s eye. These are different from the tunnels that are usually created for synthetic ICRS because they are wider and more superficial (50% depth in the author’s series). The prepared CAIRS segments are laid out flat and inserted into the tunnels with a push-in/pull-through technique using a curved Y-rod and reverse Sinskey hook. They are trimmed and positioned so that the ends lie well within the tunnel. In case cross-linking or contact lens-assisted cross-linking is being planned, the epithelium is removed (going perpendicular in the areas over the segments), the position of the segments is rechecked, and riboflavin solution is applied for half an hour followed by UV light application. A bandage contact lens is applied until epithelial healing is complete.
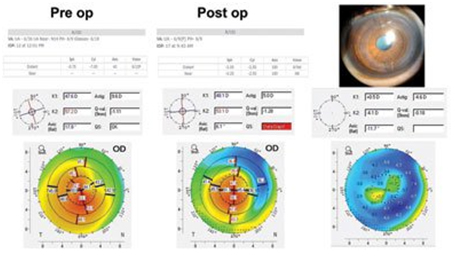
Figure 1.Postoperative slit lamp photograph after CAIRS implantation, with improvement in uncorrected visual acuity from 6/36 (20/125) to 6/9 (20/32) and best corrected visual acuity from 6/12 (20/50) to 6/9 (20/30). Decrease in refractive error, spherical equivalent, and topographic and refractive cylinder and improvement in steep and flat keratometric values are seen. Centralization of the cone and flattening and regularization of topography are seen. Difference map shows regularization and greater flattening in steepest areas.
Source: Soosan Jacob, MS, FRCS, DNB, and Amar Agarwal, MS, FRCS, FRCOphth
Mechanism
CAIRS acts as a spacer graft and thereby regularizes the corneal topography and centralizes the cone. It also helps decrease progression by redistributing corneal stress forces. It improves quantity and quality of vision, both uncorrected and best corrected visual acuity, and decreases refractive error, both sphere and cylinder. Improvement in topographic, refractive and visual parameters was seen in our published study in Journal of Refractive Surgery. Microscopic images of the CAIRS segments have shown regular even cuts and structurally unaltered normal corneal tissue, and anterior segment OCT has shown stability of the segments over time.
Advantages
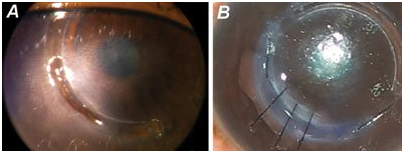
Figure 2.Post-INTACS melt (a) treated with explantation of Intacs segment and implantation of a CAIRS segment (b). The CAIRS segment fills the tissue defect as well as retains topographic effects.
Because CAIRS is made of human donor corneal stromal tissue, it shows good biocompatibility and integration into the host cornea. Unlike ICRS, it does not hinder the passage of oxygen and nutrients. It is also not associated with the presence of a hard substance within the cornea that can potentially lead to ICRS migration, host corneal necrosis and melt, or extrusion or intrusion of synthetic ICRS. Complications such as neovascularization, infections, delayed acute hydrops secondary to intrusion, refractive and topographic fluctuations due to motility of synthetic ICRS, inflammation, peri-channel deposits, pain and sensitivity have also been reported with synthetic ICRS, and CAIRS, through the use of allogenic tissue, can help avoid these.
The effect of synthetic segments is limited because they have to be implanted deep in the corneal stroma at about 70% to 80% depth. In contrast, because CAIRS is allogenic, it can be implanted more superficially, at 50% depth, thereby making it possible to achieve better effect. In addition, varying arc segments, even up to 360°, can be easily implanted with CAIRS. CAIRS also can help avoid the glare that patients with synthetic segments often experience from edge effects.
Synthetic segments cannot be implanted in very thin corneas, and a minimum stromal thickness of 450 µm in the zone of implantation is required to perform the procedure. CAIRS does not require a minimum corneal thickness, and as long as femtosecond-dissected channels can be created in the desired optic zone, CAIRS can be implanted. We are now able to perform CAIRS with cross-linking safely even in corneas that are steep but have sufficient pachymetry for contact lens-assisted cross-linking, although previously we would have done a deep anterior lamellar keratoplasty because of the cross-linking risks in such steep corneas. This is possible because the initial flattening created by the CAIRS segments makes the cornea suitable for safe subsequent cross-linking. It has thus helped prevent a corneal transplantation in many extreme cases. CAIRS has also given us equally good results in patients with early disease as well by improving the quality of vision and decreasing refractive error. Thus, in our experience, we saw that CAIRS could be applied to almost the entire range of keratoconic corneas. It may also be used to improve quantity and quality of vision in other ectatic conditions and causes for irregular astigmatism. We have also used CAIRS segments to treat melts related to Intacs (Addition Technology) and Keraring (Mediphacos). We did this by removing the synthetic ICRS causing the melt and implanting an appropriately sized CAIRS segment into the same channel. The segment is held in place in the initial postoperative period with anchoring sutures at either end and bridging sutures in the area of melt.
Conclusion
In our experience of close to 4 years, CAIRS has shown to be effective, safe, stable and simple while retaining advantages of reversibility and adjustability. It is also more economical as multiple segments can be prepared from one donor cornea, thus allowing multiple patients to be treated. Eye banks may be involved in preparation and processing of tissue. We did not notice any incidence of inflammation or stromal rejection even though patients were kept on topical steroids for only 6 weeks. This is likely to be due to the low volume of tissue transferred, only stromal and not endothelial and epithelial tissue being transferred, rapid repopulation by host keratocytes from all sides of the ensconced tissue segment, placement far from the limbus and limbal blood vessels, and a lack of sutures extending to the limbus (unlike corneal transplants). Even in the eventuality of a rejection, because the segments are outside the visual axis, they continue to provide an improvement in topography and vision.
References:
- Jacob S. CAIRS a new technique for keratoconus and corneal ecstasias. youtube.com/watch?v=qF-9ycSQPq8. PublishedMay 9, 2017.
- Jacob S. CAIRS (corneal allogeneic intrastromal ring segments) for keratoconus, ectasias & irregular corneas. youtube.com/watch?v=SkxLwgP8cXA. PublishedFeb. 24, 2019.
- Jacob S, et al. J Refract Surg. 2018;doi:10.3928/1081597X-20180223-01.
- Formoreinformation:
- Amar Agarwal, MS, FRCS, FRCOphth, is director of Dr. Agarwal’s Eye Hospital and Eye Research Centre. Agarwal is the author of several books published by SLACK Incorporated, publisher of Ocular Surgery News, including Phaco Nightmares: Conquering Cataract Catastrophes, Bimanual Phaco: Mastering the Phakonit/MICS Technique, Dry Eye: A Practical Guide to Ocular Surface Disorders and Stem Cell Surgery and Presbyopia: A Surgical Textbook. He can be reached at 19 Cathedral Road, Chennai 600 086, India; email: aehl19c@gmail.com; website: dragarwal.com.












